New Delhi: The Insurance Regulatory and Development Authority of India (IRDAI) has issued a stern warning to general and health insurance companies to stop publishing misleading advertisements about claims settlement ratios. According to the regulator, there is a significant gap between what insurance companies claim in ads and the actual reality of settlements.
Misleading Claims Settlement Ratios
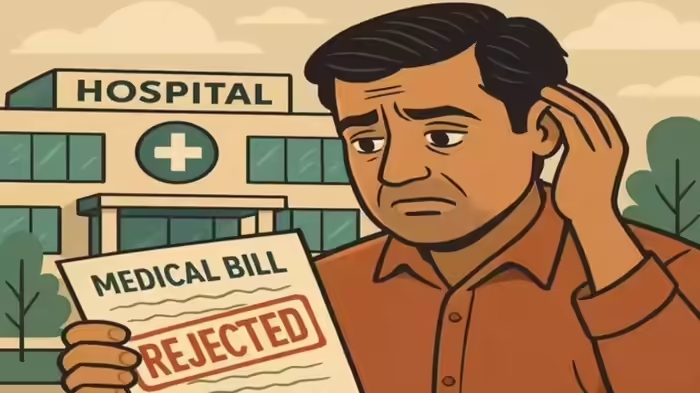
IRDAI observed that many insurance companies present their claims settlement ratios in a misleading and deceptive manner, making it appear as though very few claims are rejected, while the actual figures submitted to the regulator tell a different story. Companies often use different definitions to calculate settlement ratios and exclude rejected or pending claims in their advertisements. These numbers frequently do not match the audited figures in their annual reports.
Regulator’s Instructions to Insurance Companies
The IRDAI has directed insurers to review their current practices, identify gaps, and adopt a standardized formula for calculating claims settlement ratios. This formula should be applicable across all insurance types, including motor, health, personal accident, fire, and marine insurance. The goal is to establish a uniform benchmark for the entire insurance industry.
Reasons for Claim Rejections
Insurance companies explained that claims may be rejected due to missed document submission deadlines or because certain claims do not meet contractual terms.
Guidance for Customers
The regulator emphasized that policyholders should not focus solely on settlement ratios. They should also consider:
- Claim processing time
- Reasons for claim rejections
- Overall quality of claim services
Once a standardized approach is adopted, these factors will be assessed consistently across the industry.
Key Statistics (FY 2023-24)
- 83% of claims settled
- 11% of claims rejected
- 6% of claims pending as of 31 March 2024
- ₹2.69 crore in health insurance claims settled
- ₹83,493 crore total paid by insurers for claims
Financial Impact
Due to inefficiencies and malpractices in the insurance sector, an estimated ₹10,000 crore is lost annually. IRDAI highlighted the urgent need for insurers, government, and regulators to collaborate to maintain public trust in the sector.
Discover more from SD NEWS agency
Subscribe to get the latest posts sent to your email.